Individual results may vary
"During an AHP attack—you’re in so much pain, you can barely walk. But no one can see it."
—Amalia, an artist and Alnylam Patient Ambassador on GIVLAARI

Individual results may vary
"During an AHP attack—you’re in so much pain, you can barely walk. But no one can see it."
—Amalia, an artist and Alnylam Patient Ambassador on GIVLAARI

What is acute hepatic porphyria (AHP)?
AHP is a family of rare, genetic diseases that can cause severe and potentially life-threatening attacks. Some people with AHP also have chronic, debilitating symptoms when they are not having an attack.
There are 4 types of AHP:
- Acute intermittent porphyria (AIP)
- Hereditary coproporphyria (HCP)
- Variegate porphyria (VP)
- ALAD-deficiency porphyria (ADP)
- Acute intermittent porphyria (AIP)
- Variegate porphyria (VP)
- Hereditary coproporphyria (HCP)
- ALAD-deficiency porphyria (ADP)
ALAD=delta-aminolevulinic acid dehydratase.
How AHP affects the body
In people with AHP, the heme production process in the liver does not work properly because of a genetic mutation. In the liver, this process is controlled by an enzyme called delta-aminolevulinic acid synthase 1 (ALAS1).
There are certain triggers that can activate ALAS1. Some known triggers include hormonal fluctuations, infection, stress, use of certain medications, alcohol consumption, and fasting/low-carbohydrate diets.
When ALAS1 is activated, the heme production process is unable to keep up. This causes toxic substances called delta-aminolevulinic acid (ALA) and porphobilinogen (PBG) to build up. ALA and PBG are associated with attacks and other AHP symptoms.
In AHP, when ALAS1 is activated in the liver the heme production process is unable to keep up.
This causes toxins ALA and PBG to build up in the liver and be released throughout the body.
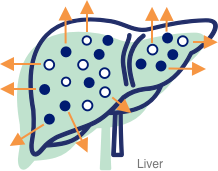
ALA
PBG
ALA and PBG are associated with attacks and other AHP symptoms.